Remember your purpose and your core beliefs when your authority or expertise is challenged. As Christ never wavered in his belief and desire to cast out demons, even if others were skeptical, so must be also have the trust and confidence in our desire to do what is best.
The Gastrointestinal Tract and Palliative Care
Let food be thy medicine
(Hippocrates)
It is the time of the year again when we indulge on food. The Christmas Holidays bring out the foodie in all of us, whether as a chef or as a food critic. Food is given as a gift, plays a central role in family and class reunions, and can make or break any gathering among friends and relatives. But is food and gastrointestinal nutrition also important for palliative and hospice patients?
One of the most neglected aspects of chronic care is nutrition. We are sometimes too focused on curative modalities involving drugs and procedures. Recovery from illness and improving the quality of life entails attention to gastrointestinal health and nutrition, for it allows the body to extract vitamins and minerals that will allow natural healing. Evidence shows that there are better outcomes when adequate nutrition is combined with medications.
The gastrointestinal (GI) tract is a complex system that plays a critical role in our overall health, particularly for individuals with chronic illnesses. A healthy GI tract is essential for processes such as nutrient absorption, immune response, and even mental health, all of which can significantly influence the management and progression of chronic conditions. (1)
At the core of a healthy GI tract's contribution to managing chronic illness is its role in nutrient absorption. The intestines are responsible for breaking down food into its constituent nutrients—vitamins, minerals, fats, carbohydrates, and proteins—that the body requires for energy, growth, and repair. For patients with chronic illnesses, deficiencies in these nutrients can exacerbate their conditions. Conditions like rheumatoid arthritis or inflammatory bowel disease (IBD) can lead to malabsorption issues and nutritional deficiencies, which may worsen inflammation and symptoms. A healthy gut can facilitate better absorption of anti-inflammatory nutrients such as omega-3 fatty acids, vitamins C and E, and other antioxidants.
The GI tract is also vital for effectively managing blood sugar levels. A diet rich in fiber, which promotes a healthy gut microbiota, can lead to improved insulin sensitivity and better blood glucose control.
Individuals with heart disease can benefit from the absorption of heart-healthy nutrients, such as potassium and magnesium, through a well-functioning GI tract, while also obtaining dietary fiber to manage cholesterol levels.
The GI tract houses about 70% of the body’s immune system. A healthy gut influences immune function via the gut-associated lymphoid tissues (GALT), which contain immune cells ready to respond to pathogens. For patients with chronic illnesses—especially those involving autoimmunity or chronic inflammation—the ability to modulate immune responses is particularly important. Conditions such as lupus or multiple sclerosis (MS) are characterized by an overactive immune response. A balanced gut microbiome, supported by a healthy diet rich in probiotics and prebiotics, can help regulate immune responses and reduce inflammation. This balance can also lower the incidence of autoimmune reactions, allowing for better management of symptoms.
For patients with chronic infections like HIV or those undergoing treatments that compromise the immune system, a healthy GI tract can improve overall health by ensuring adequate nutrient intake and facilitating gut health. This strengthens the immune response and may delay the progression of disease.
Emerging research emphasizes the gut-brain connection—how the state of the GI tract can influence mental health, mood, and cognitive function. Chronic illnesses often come with psychological challenges, including depression and anxiety. The gut microbiota produces neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which are crucial for mood regulation. Individuals with healthy gut flora often experience better mental wellbeing, which is essential since chronic illness can lead to stress and mental health challenges. (2)
Chronic stress can negatively impact gut health, leading to a vicious cycle where poor GI function exacerbates stress and anxiety. A healthy gut can improve resilience to stress and reduce anxiety levels.
Chronic inflammation is a hallmark of many illnesses, contributing to disorders such as diabetes, cardiovascular disease, and even certain types of cancer. To manage chronic inflammation, a healthy GI tract plays a pivotal role. Consuming a diet rich in whole foods, fiber, and fermented products can support a healthy gut microbiota. Foods like fruits, vegetables, whole grains, and probiotics (e.g., yogurt, sauerkraut) can help foster beneficial bacteria that combat inflammation. When fiber is fermented in the gut, it produces Short Chain Fatty Acids (SCFAs), such as butyrate, which can reduce systemic inflammation, fortify the gut barrier, and prevent the entry of harmful substances into the bloodstream. (3)
The GI tract also houses a significant part of the endocrine system. Hormonal balance is crucial in managing chronic illnesses, and a healthy gut plays a role in this balance.
Gut health can influence insulin sensitivity. A balanced microbiome can decrease insulin resistance, which is particularly beneficial for managing diabetes and obesity. Conditions like Hashimoto's thyroiditis highlight the interplay between gut health and endocrine function. The absorption of iodine and selenium—essential for thyroid health—depends on a well-functioning GI tract.
Digestive issues such as bloating, constipation, and diarrhea are common in chronic illness. These symptoms can detract from the quality of life and complicate disease management. Dietary adjustments that enhance gut health, such as increasing fiber intake and staying hydrated, can alleviate digestive symptoms. This, in turn, may improve adherence to treatment protocols and dietary recommendations that benefit overall health. A healthy GI tract maintains its barrier integrity, preventing leaky gut syndrome, where toxins and undigested food particles enter the bloodstream. This syndrome has been linked to various chronic illnesses such as autism, celiac disease, and inflammatory diseases.
For patients with chronic illness, nurturing a healthy gastrointestinal tract can lead to profound beneficial outcomes. Improved nutrient absorption, better immune system function, enhanced mental health, reduced inflammation, hormonal balance, and improved digestive function all contribute to a more effective management of chronic diseases. Thus, focusing on gut health through diet, lifestyle changes, and possibly probiotics can help improve not only quality of life but also the overall management of chronic health conditions. Ultimately, fostering a healthy gut can be a cornerstone strategy in the holistic management of chronic illness.
REFERENCES
Primary Health Care. 21, 6, 48-56. doi: 10.7748/phc.21.6.48.s15
Back to the future of psychoneuroimmunology: Studying inflammation-induced sickness behavior, Brain, Behavior, & Immunity - Health, Volume 18,2021, 100379, ISSN 2666-3546, https://doi.org/10.1016/j.bbih.2021.100379
Blaak, E.E., E.E. Canfora, S. Theis, G. Frost, A.K. Groen, G. Mithieux, A. Nauta, K. Scott, B. Stahl, J. van Harsselaar, R. van Tol, E.E. Vaughan, and K. Verbeke. "Short chain fatty acids in human gut and metabolic health". Beneficial Microbes 11.5 (2020): 411-455
Colorectal Cancer
Colorectal cancer, also known as bowel cancer or colon cancer, is a type of cancer that starts in the colon or rectum. The colon and rectum are parts of the large intestine, which is responsible for the final stages of digestion and elimination of waste. Colorectal cancer usually begins as a growth called a polyp on the inner lining of the colon or rectum, which can eventually develop into cancerous cells.
Colorectal cancer is one of the most common types of cancer worldwide, and its risk increases with age. Symptoms of colorectal cancer may include changes in bowel habits (such as diarrhea or constipation), rectal bleeding, blood in the stool, abdominal discomfort or pain, unexplained weight loss, fatigue, or weakness. However, these symptoms may also be caused by other conditions, so it is important to consult a healthcare professional for a proper diagnosis.
Regular screening through methods like colonoscopy can help detect colorectal cancer early when it is easier to treat and cure. Treatment options for colorectal cancer may include surgery to remove the tumor, chemotherapy, radiation therapy, targeted therapy, or a combination of these approaches, depending on the stage and extent of the cancer. As with any cancer, early detection, prompt medical intervention, and lifestyle modifications such as a healthy diet and regular exercise can help in prevention and management.
Colorectal cancer can be dangerous for several reasons:
1. Late diagnosis. Often, colorectal cancer is not diagnosed in its early stages because it can develop slowly without causing noticeable symptoms. As a result, the cancer can progress to advanced stages by the time it is detected, making it more challenging to treat.
Colorectal cancer may not exhibit obvious symptoms in its early stages, leading to delayed medical attention. By the time symptoms like unexplained weight loss, rectal bleeding, or changes in bowel habits appear, the cancer may have already progressed.
2. Metastasis or spread. Colorectal cancer has the ability to spread or metastasize to other parts of the body, such as the liver, lungs, or lymph nodes. This can occur when cancer cells from the colon or rectum break away and travel through the bloodstream or lymphatic system. Metastatic colorectal cancer is more difficult to treat and is associated with a poorer prognosis.
3. Obstruction and perforation. As colorectal tumors grow in size, they can obstruct or block the digestive tract, causing symptoms like abdominal pain, constipation, or bowel changes. In some cases, the tumor can perforate or tear through the wall of the colon or rectum, leading to infection and potentially life-threatening complications.
4. High recurrence rates. Even after successful treatment, colorectal cancer has a higher risk of recurrence compared to some other types of cancer. This underscores the importance of ongoing surveillance and follow-up care to detect any potential recurrence early.
5. Limited treatment options. Depending on the stage and characteristics of the cancer, treatment options for colorectal cancer may include surgery, radiation therapy, chemotherapy, and targeted therapy. However, advanced or metastatic colorectal cancer can be challenging to treat, and in some cases, treatment may only be able to control the disease rather than cure it completely.
Therefore, it is essential to be aware of the potential risks and take proactive measures, such as routine screenings, to detect and treat colorectal cancer in its early stages for a better prognosis.
There are several measures individuals can take to help prevent colorectal cancer:
1. Regular screenings. One of the most effective ways to prevent colorectal cancer is to undergo regular screenings. These screenings can detect precancerous growths or early-stage cancers, allowing for timely intervention and treatment. The most common screening test is a colonoscopy, which is typically recommended starting at age 45 or earlier for individuals with a family history of the disease.
2. Healthy diet. Maintaining a balanced and nutritious diet can lower the risk of colorectal cancer. Focus on consuming plenty of fruits, vegetables, whole grains, and lean proteins while minimizing the intake of processed and red meats. Avoiding excessive consumption of sugary drinks, alcohol, and foods high in fat can also be beneficial.
3. Regular physical activity. Engaging in regular physical activity, such as brisk walking, jogging, swimming, or cycling, can help decrease the risk of colorectal cancer. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous exercise each week.
4. Limit alcohol consumption. Excessive alcohol consumption has been linked to an increased risk of colorectal cancer. Limit alcohol intake to moderate levels, which means up to one drink per day for women and up to two drinks per day for men.
5. Avoid tobacco. Smoking has been associated with an increased risk of various cancers, including colorectal cancer. Quitting smoking or avoiding tobacco products altogether can significantly reduce the risk of developing colorectal cancer.
6. Maintain a healthy weight. Being overweight or obese increases the risk of colorectal cancer. Strive to achieve and maintain a healthy weight through a balanced diet and regular physical activity.
7. Increase fiber intake. Consuming foods high in fiber, such as whole grains, legumes, fruits, and vegetables, can help reduce the risk of colorectal cancer. Aim for at least 25-30 grams of fiber daily.
Remember, while these preventive measures can lower the risk, they do not guarantee complete prevention of colorectal cancer. It is crucial to stay vigilant, undergo recommended screenings, and seek medical attention if any concerning symptoms arise.
Understanding Palliative and Hospice Care in the Philippines
There is an end to cure; there is no end to care.
Palliative and hospice care plays a crucial role in improving the quality of life of patients with life-limiting illnesses. This specialized form of care focuses on providing relief from the symptoms, pain, physical stress, and mental anguish associated with serious illnesses. While the concept of palliative and hospice care is gaining recognition worldwide, its understanding and implementation in the Philippines remains limited.
Despite efforts to improve access to these services, the majority of Filipinos do not have access to quality palliative and hospice care. A study conducted by Erfe and colleagues in 2020 revealed that only 10% of hospitals in the country have palliative and hospice care units. Moreover, the same study found that there is a significant lack of specialized healthcare professionals trained in palliative and hospice care.
A number of challenges hinder the development and implementation of palliative and hospice care. There is a perceived lack of awareness among the general population and even healthcare professionals about palliative and hospice care. Some doctors do not want to refer their patients to a palliative care specialist because they believe it means giving up and failing as a physician. Many people mistakenly believe that these forms of care are synonymous with end-of-life care or euthanasia, leading to reluctance in seeking or providing such services.
The shortage of trained healthcare professionals in palliative and hospice care results from the limited inclusion of palliative and hospice care in medical education. As a result, healthcare professionals often lack the skills and knowledge necessary to provide comprehensive palliative and hospice care to patients in need. The number of questions about palliative and hospice care principles in the physician licensure exam is very limited if we think of its applicability in the medical field where treatment failure at the end of life is inevitable.
The limited availability of resources is another major challenge. Palliative and hospice care requires the maintenance of specialized facilities, access to various medications for pain management, and support from allied health professionals such as psychologists and social workers. However, these resources are lacking in many healthcare institutions, making it difficult to provide comprehensive care to patients. The simple provision of pain-modifying opioids, even in large institutions, is lacking, making patients bear with pain and suffering for prolonged periods.
Cultural and religious factors also contribute to the slow implementation of palliative and hospice care in the country. Filipinos have a strong familial and religious support system, which can sometimes conflict with opting for palliative and hospice care. Many families prefer to care for their loved ones at home, with the belief that it is their duty to do so. This cultural norm limits the acceptance and utilization of palliative and hospice care services.
There are several potential avenues for improving palliative and hospice care in the Philippines.
Firstly, increasing awareness through education campaigns and public discourse is crucial. Efforts should be made to educate the general population, healthcare professionals, and policymakers about the nature and benefits of palliative and hospice care. This can help dispel misconceptions and foster a more accepting attitude towards these services.
Secondly, incorporating palliative and hospice care into medical education curricula can contribute to the availability of well-trained healthcare professionals. The Philippine government and medical schools should collaborate to include relevant coursework and training in palliative and hospice care to ensure that future healthcare professionals are equipped with the necessary skills.
Addressing the resource shortage issue requires both financial and institutional support. The government should allocate funds specifically for the development and maintenance of palliative and hospice care units in hospitals and healthcare institutions. Additionally, expanding the availability and accessibility of pain management medications is imperative to ensure that patients receive optimal relief from their symptoms.
Cultural and religious factors should be taken into account when designing palliative and hospice care services. Collaborating with local community leaders, religious organizations, and healthcare professionals can help bridge the gap between traditional and modern care approaches. By involving the community in the decision-making processes, a more culturally sensitive approach can be developed.
Despite the challenges faced by palliative and hospice care in the Philippines, there is a growing need for these services to improve the quality of life for patients with life-limiting illnesses. By increasing awareness, providing comprehensive education, allocating resources, and addressing cultural and religious concerns, palliative and hospice care can be better understood and implemented. The development and improvement of these services are not only essential for improving patient care but also for the overall well-being of families and society.
Pediatric Palliative Care: Addressing the Complex Needs of Children
One of the most difficult services to find in the Philippines is the provision of Pediatric Palliative Care. While there is a growing recognition of its significance in the past decade, integrating Pediatric Palliative Care into the healthcare system and providing access to it needs to improve. There is a need for a specialized medical approach that provides comprehensive comfort and support to children with serious illnesses and their families. It is care that focuses on addressing the physical, emotional, social, and spiritual needs of children with life-threatening conditions. It emphasizes improving the quality of life for these patients through pain and symptom management, communication, and coordination of care. Goals of pediatric palliative care often include enhancing the child's comfort, ensuring shared decision-making, reducing hospital readmissions, and providing grief support to the family.
Pediatric Palliative Care must be employed throughout the continuum of care for children with serious illnesses, and it must be introduced early enough to enable better outcomes. It can actually be introduced at any stage of the illness and can be provided alongside curative treatments. Palliative care teams work collaboratively with medical professionals, parents, and other relevant individuals to develop an integrated care plan tailored to the child's unique needs. Services may include pain management, psychosocial support, skilled nursing care, respite care, bereavement support, and counseling.
The improved health outcomes of Pediatric Palliative Care are due to its strong focus on managing pain and other distressing symptoms that can significantly improve a child's overall well-being. It is care that is holistic. It addresses the physical, emotional, social, and spiritual dimensions of the child's life, helping to reduce suffering. This results in a better quality of life for both the child and their family.
Pediatric palliative care recognizes the importance of supporting the family and aiding access to community resources. Social workers work hand in hand with physicians and nurses to provide emotional and psychosocial support and facilitate communication and decision-making. This is especially important for patients who are not that well-off financially.
The palliative care team collaborates with the child's primary healthcare providers and other specialists, ensuring seamless transitions between care settings. At every stage of the illness trajectory, support is available. It encourages open and honest conversations about the child's illness, prognosis, and treatment options, empowering families to make well-informed decisions.
However, many families face challenges in accessing pediatric palliative care due to geographic or financial barriers, lack of awareness, or shortages of healthcare professionals trained in pediatric palliative care. Palliative care can also bring up emotional and existential challenges for families, particularly when discussing end-of-life matters, which can be overwhelming for some. Some healthcare providers may have limited understanding or training in pediatric palliative care, leading to misconceptions or discomfort in initiating discussions.
The field of pediatric palliative care continues to evolve and grow. It is anticipated that there will be increased awareness and integration of palliative care principles into various settings, including primary care practices and hospitals. Developing innovative approaches, such as telemedicine and mobile health technologies, may help bridge the gap in accessing palliative care for remote or underserved populations. Additionally, advancements in research and education are essential to improve the effectiveness, accessibility, and quality of pediatric palliative care.
Pediatric palliative care aims to improve the quality of life for children with serious illnesses while providing comprehensive support to their families. Addressing physical, emotional, social, and spiritual needs offers a holistic approach to care. While challenges exist, ongoing efforts to increase awareness, improve access, and advance research hold promise for the future of pediatric palliative care, ensuring that children and their families receive the support they need during challenging times.
SURVIVING NEGATIVITY
“Optimism is the one quality more associated with success and happiness than any other.”
Brian Tracy
It is a challenging and crazy world. But we continue to exist.
I heard a friend tell me that to live in this world is to survive. There are always obstacles to hurdle, and once we get over it, we move on to the next. The walls to traverse may differ between us, but the wall is there - imposing its will. Those walls will not move, so we must move it, tear it down, or pass through. The decision on what to do ultimately rests in us.
Recently, we have seen how anger can rear its ugly head when provoked by the way of road rage. Humans are triggered by perceived impartiality or inequality, or when a lack of respect is felt. In a perfect world, these would be easy to brush off, but we are not in a perfect world. We also know that not all of us are gifted with the traits of patience and understanding, so we always need to work on managing our emotions.
To help us make decisions (yes, ultimately, our reactions are a result of our decisions), our thoughts need to be conditioned to neutralize or even eliminate negativity. It is said that humans have this natural tendency to put themselves down and think negatively, so there has to be a conscious effort to resist this inclination.
What, therefore, is the mindset of a positive individual, and how can we adopt it?
First, we must avoid negativity. Even in the hour of death, as we face sickness and disease, we must look at the bright side. A suffering individual may find reprieve from a long history of pain and discomfort when the time comes to leave. Shunning negative thoughts does not mean indifference – it conveys a recognition that not all is lost for there are still people who love and need us.
Second, our words lead us to our emotions. When we fill our language with positivity and good vibes, positivity seeps into our consciousness and uplifts others. We are then strengthened by the goodness around us, even in moments of grief and despair. This is why when a loved one is lost, we give our condolences and render words of encouragement.
Third, we must remain grateful. In the face of loss, we find things that we have. Family, friends, a roof to sleep under, and a job allow us to offset whatever we lack in physical attributes, financial stability, and talent. Thankfulness also means being able to pay it forward. We must actively search for opportunities to be a blessing to others, so we see that our miseries can be handled with ease.
Fourth, our health must be at its best so that we can do and achieve more. Nothing dampens a day more than having uncontrolled pain and unmanageable symptoms. We must also exert effort to minimize pain and discomfort for others. If health problems cannot be prevented, at the very least, they must be managed well through proper diet, exercise, and medications.
Lastly, find positive, well-meaning people. These are individuals with the same thrust as ours – to help and be a positive influence. Counseling others to limit negativity is also imperative. Seek to make a happy community that uplifts and energizes so you will not see the dark side of the day.
Rekindle optimism, and spread good vibes!
PALLIATIVE CARE BENEFITS IN CANCER CARE
"I implore people to check out hospices - if you've got the choice to use them, then use them. It's not all doom and gloom."
- Jonnie Irwin, lung cancer patient
About 1.7 million people die of lung cancer each year (1). It accounts for about 1/5 of all cancer-related deaths worldwide. Palliative care is medical care aimed at improving the quality of life of seriously ill patients. While it does not have the goal of providing curative treatment in all cases, its principle lies in improving quality of life and providing comfort. The holistic nature of palliative care also ensures that it is not just physical symptoms that are addressed, but the psychosocial aspect of disease as well.
Previous studies have been done to determine the actual benefits of palliative care. In lung cancer, palliative care improves patient and caregiver outcomes and is also associated with fewer medical interventions near the end of life (2). Healthcare costs and utilization are also improved (3). Palliative care is associated with decreased cost, and as the clinical and economic benefits of palliative care for metastatic cancer patients become evident, more patients are seeking treatment (4).
What specific benefits does palliative care provide for cancer patients? Research has shown that there are benefits for the patients in the following aspects: symptom management, knowledge of the disease, and holistic approach.
Some of the common physical manifestations of cancer include pain, anorexia, cachexia, fatigue, nausea, constipation, dyspnea, and malignant bowel obstructions. These physical symptoms as well as the related spiritual and psychosocial distress during a patient's treatment course are routinely addressed by physicians. Recent clinical studies that measure patient feedback and patient-reported outcomes have shown an added clinical benefit, empowering patients to participate in decision-making and allowing for earlier detection of symptom recurrence. It has been demonstrated that patients initiating chemotherapy who are trained to notify their healthcare teams with interval symptoms have a higher quality of life and improved overall survival compared with patients who receive usual care (5).
In comparison to patients who never participated in or only had minimal conversations about disease outcomes with their physicians, patients involved in treatment planning had higher illness understanding scores and better insight into the terminal nature of cancers. In addition, conveying information with compassion correlates with patients' satisfaction with care, as content presented in a more optimistic manner is often associated with higher levels of perceived physician expertise.
It is now common knowledge that systemic chemotherapy without a clear benefit for patients at the end-of-life results in excessively toxic outcomes. Delayed referral to hospice and palliative care may not improve survival, but it may improve patient outcomes in terms of quality of life (6). Given the proven value of palliative care in oncology for symptom management, quality of life, and prognostic understanding of terminal illnesses, there has been growing evidence in the last decade to support the early provision of palliative care for cancer patients in general, not just for lung cancer.
The median survival of patients randomized to early palliative care was 11.6 months, whereas the median survival of patients receiving standard oncologic care alone was 8.9 months (p = 0.02). Patients assigned to early palliative care also received less aggressive cancer-directed care, including chemotherapy, at the end of life (7). Thus, not only does palliative care prolong survival in some cases, but it also results in the removal of unnecessary treatment modalities that may increase management costs. While some may view referral to palliative care as an added expense, studies tend to prove otherwise, as the benefits far outweigh the increased initial cost of palliative care referral.
With the advent of Universal Health Care, and in conjunction with Republic Act 11036 or the Mental Health Act for providing mental health facilities in the community, palliative care must also be provided on a larger scale. The physical and psychosocial aspects of illness could be better addressed with early referral and management. It could mean the difference in terms of overall health outcomes.
REFERENCES
1. Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2016;388:1459–544.
2. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2010;363:733–42.
3. Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993;328(15):1092–6.
4. Huo J, Hong YR, Turner K, Bian J, Grewal R, Wilkie DJ. Utilization pattern and service settings of palliative care for patients with metastatic non-small cell lung cancer. Cancer. 2019;125(24):4481–9.
5. Basch E, Deal A M, Kris M G et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. 2016;34(06):557–565.
CARETAKERS
I expect to pass through this world but once; any good thing therefore that I can do, or any kindness that I can show to any fellow-creature, let me do it now; let me not defer or neglect it, for I shall not pass this way again.
Stephen Grellet
As human beings with advanced knowledge, several vital tasks are incumbent upon us in order to take care of our planet. For example, we have to sustain each species that walks the earth and ensure that they continue to exist. While it is not given to everyone to go about being botanists and veterinarians, all of us, regardless of circumstances, are called to be caretakers. We have to take care of one another because losing a species could have serious ecological consequences. Biblically, we were all tasked with this function. And in a practical sense, only humans can really assume this responsibility.
The power to serve as a caretaker is a gift. Our intelligence and ability to become stewards not only rest in our ability to communicate. Our higher order skills – the ability to manipulate the environment – are seen in our upright posture (to see the horizon unlike other animals), our opposable thumb in our hands (to handle tools), and the larger brain in proportion to body size (to process information) may not be enough for us to protect ourselves, but they make us more creative in seizing opportunities. We may not be the strongest, fastest, or largest animals, but we certainly have the greatest capacity for adaptation and intellectual growth. Humans, to a certain extent, may be helpless in the face of certain calamities, but we can certainly predict them better and do something before or after these calamities occur. We populated the earth because of wisdom, grit, and resilience.
As it has been our duty to care for all living creatures, there is even more impetus for us to take care of our own. Other animals have these same caring instincts. When someone gets sick or disabled, those who are capable will search for ways to find a cure. Parents protect their families from harm and facilitate growth and development. When parents age, the roles are reversed, but at times we forget that nature takes its toll. In our desire to heal and restore, we forget to care and look inwardly to meet our needs. This is where we must draw the line and enable reason to prevail.
Social beings have this need to be accepted and respected by peers. There is, unfortunately, no medal to be gained by letting nature take its course. This makes Hospice Care quite difficult to accept for such an intelligent organism tasked to be the caretaker of nature. It takes a special breed of people with enough experience to see through nature’s limitations and say where enough is enough. This does not equate with a lack of love or nurturing or an easy surrender. If immortality were to become the norm, there is no question that the practice of hospice care would become obsolete. If we had spare parts available to replace aging ones, the concept of surrender would be deemed taboo.
There has been a great effort to find ways to keep our bodies running indefinitely. Science has made tremendous strides toward human research on artificial intelligence, artificial organs, transplant technologies, and anti-aging mechanisms. Our life expectancy is increasing, and the quality of life envisioned at the age of 60 has made retirement somewhat of a golden age. Add to that social media postings of 80-year-olds playing a good round of golf and attending to their grandchildren, and we see how the pressure mounts among us to keep our bodies alive. Extremes in life expectancies are not the norm and cannot be realized in all cases.
Individuals will continually search for ways to live longer. It is a noble endeavor. But more importantly, each must add meaning to those years by being stewards of health and well-being. We will only pass by once. Let us make the most out of it, no matter how long or short it may turn out to be.
THE IMPORTANCE OF PALLIATIVE CARE NURSING
"You matter because you are you, and you matter to the end of your life. We will do all we can not only to help you die peacefully, but also to live until you die."
— Dame Cicely Saunders, nurse, physician and writer, and founder of the modern-day hospice movement
A small percentage of persons with advanced disease die at home. However, one major limitation to carrying out this final wish is the lack of access to palliative care at home and the lack of nursing expertise to help patients during the final days. Studies indicate that nurses play a substantial role in hospice and palliative care, but the perception of the public is that they are not capable. Another issue is the reduced comfort level and negative attitude toward providing care for patients and their families at the end of life. Studies identify a lack of end-of-life care knowledge and skills among both newly graduated and student nurses. This is why providing nursing education is of paramount importance.
The Ruth Foundation meets this need for upgrading the confidence of nurses in providing Hospice and Palliative Care by providing ELNEC* (End-of-Life Nursing Education Consortium) locally. Included in the program is an Introduction to Palliative Nursing, Pain Management, Symptom Management, Communication, Ethical & Legal Issues, Cultural Considerations, Loss/Grief/Bereavement, and Final Hours. In addition, participants learn from role plays and case study reviews where they had opportunities to explore ways to improve self-care.
One of the most crucial aspects of palliative care for nurses is the ability to manage pain and other related symptoms in patients. Palliative nurses should be knowledgeable in identifying and assessing symptoms, as well as administering medications and other non-pharmacological interventions to alleviate discomfort.
Palliative nurses must be able to communicate effectively with patients and their families, as well as liaise with other healthcare professionals to ensure a coordinated approach to patient care. They should be skilled in providing support and counseling to patients and their families during end-of-life care.
A Palliative Care nurse should have a deep understanding and respect for cultural and spiritual beliefs, practices, and traditions. This is important as end-of-life choices can be influenced by cultural factors, and any misunderstandings can lead to distress for patients and their families.
Another essential aspect of end-of-life care involves care planning and coordination. Palliative care nurses should collaborate with other healthcare professionals and the patient’s family to develop personalized care plans to ensure the provision of high-quality care.
There are many ethical dilemmas in the course of palliative care nursing practice, especially surrounding issues of life-prolonging treatments and end-of-life decisions. Palliative nurses should have a strong grounding in ethical principles and should be able to apply them to clinical scenarios.
Lastly, Palliative Care nurses often encounter emotional and psychological challenges in their duties, which can leave them vulnerable to burnout and other negative outcomes. Self-care is critical to ensure that nurses remain emotionally resilient and competent in their roles.
The ELNEC curriculum has all the resources needed to empower palliative care nursing practitioners to take back to train others. There are also wonderful opportunities to network with others who are committed to improving care for all patients with life-limiting illnesses.
The most recent ELNEC Core held at The Medical City—South Luzon last April 28,2023.
* The End-of-Life Nursing Education Consortium (ELNEC) Project is a national and international end-of-life/palliative care educational program administered by City of Hope (COH) designed to enhance palliative care in nursing. Materials are copyrighted by City of Hope and the American Association of Colleges of Nursing (AACN) and are used with permission.
REFERENCES:
Fischer S, Min SJ, Cervantes L, Kutner J. Where do you want to spend your last days of life? Low concordance between preferred and actual site of death among hospitalized adults. J Hosp Med 2013;8(4):178–183.
American Association of Colleges of Nursing. End-of-Life Nursing Education Consortium (ELNEC) fact sheet 2016. American Association of Colleges of Nursing Website.
Von Ah D, Cassara N. Perceptions of cultural competency of undergraduate nursing students. Open J Nurs 2013;3(2):182–185.
THE PALLIATIVE CARE NETWORK (PCN): A MODEL FOR LOCAL HEALTH CARE
The multidisciplinary nature of Palliative and Hospice Care makes health care integration and local government support an important facet in improving the health of the people.
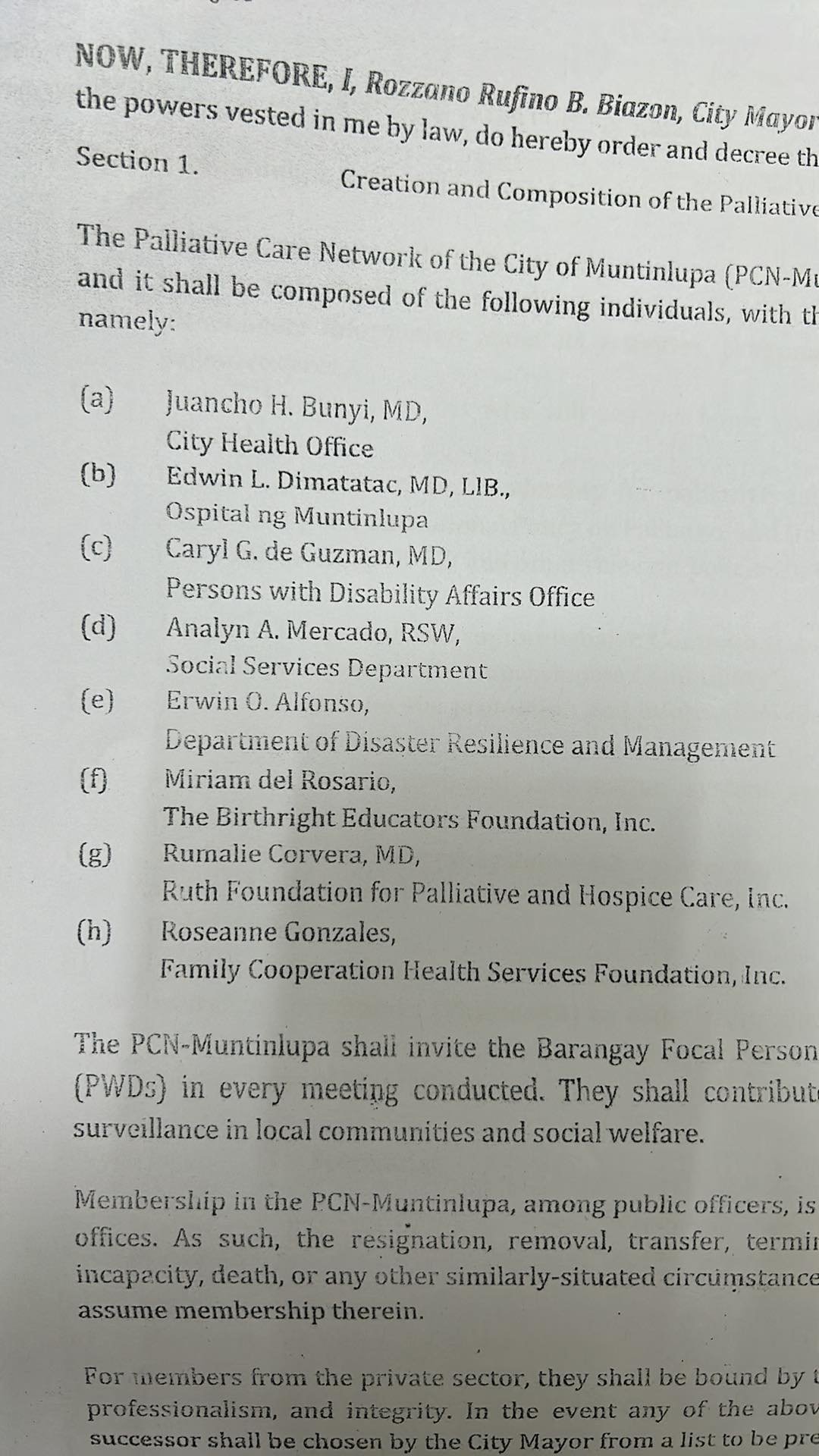
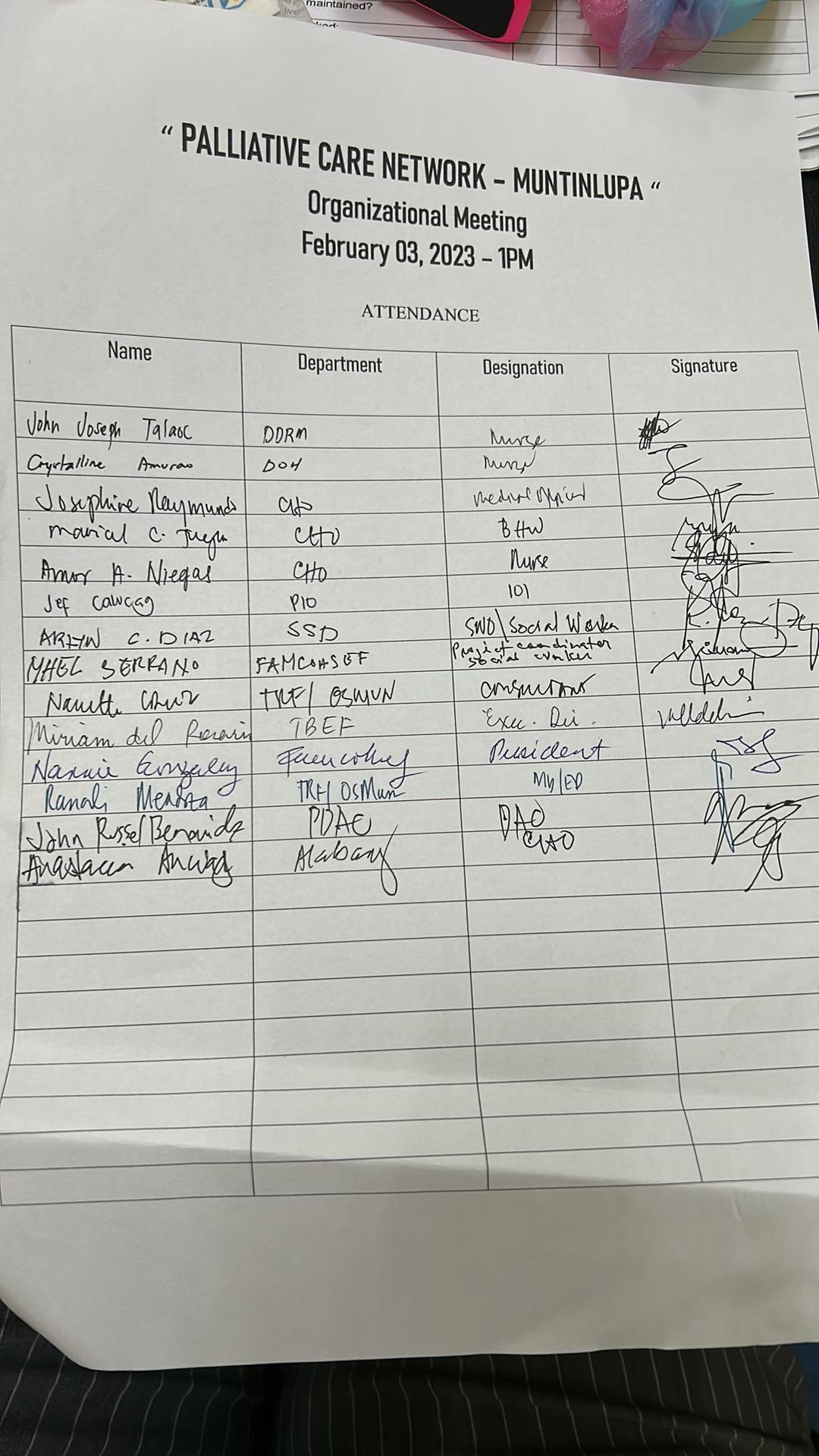
With the aim of providing health programs on primary health care, the City of Muntinlupa, in partnership with The Ruth Foundation for Hospice and Palliative Care (TRF), has created the Palliative Care Network (PCN). As approved by Muntinlupa City Mayor Rozzano Rufino “Ruffy” Biazon, PCN-Muntinlupa will be headed by its Chairperson, Dr. Juancho Bunyi (City Health Officer) with the participation of TRF CEO Dr. Rumalie Corvera, as one of its members.
PCN Muntinlupa will act as a sounding board for the provision of palliative care services in the city. Activities, programs, and training related to palliative care are expected to be put into place. It is also imperative that patient visits be conducted at home for those without the capability to travel to healthcare facilities.
To build a compassionate community rooted in scientific processes, PCN will also push for more evidence-based research on hospice and palliative care that will be published in peer-reviewed journals. The referral system is also going to be streamlined to create a more viable network for care provision and to lessen the stress of caregivers and families when trying to access care for their relatives with chronic illnesses. This will also be lined up with the comprehensive benefits package for Palliative Care in the Philippine Health Insurance Corporation.
The outcomes that can be expected from this network are immeasurable. It may not produce income, but it will create a more productive workforce that can focus on its economic needs instead of worrying about where to bring a relative who needs palliative care. A compassionate community encourages more empathy among its constituents, rekindling the “bayanihan” spirit of the Filipino where neighbors and friends help out in whatever capacity when someone is in need. Government officials would find more purpose in their activities, seeing that they make a difference in the lives of their constituents through hospice care. Businesses would create more socially relevant projects for palliative care and contribute their resources to generate goodwill. Religious leaders would find in hospice and palliative care a way to live out their teachings and provide counselling and support for those in distress.
In due time, PCN hopes that it can create a template that can be duplicated in other cities and municipalities. The Universal Health Care Law aims to provide Filipinos access to quality and cost-effective care. With proper planning, resource allocation, sound leadership, and determination to succeed, even those without the means to afford medical services can be given a life filled with dignity and hope. Local governments would also be able to instill a culture that is rooted on healthy lifestyles, disease prevention, and scientific management of disease and illness.
We would like to congratulate the City of Muntinlupa and The Ruth Foundation for its participation in this network. It is part of every individual’s vision to live a life that cultivates care and compassion. In the end, it is what makes us human. No amount of success and wealth can ever compensate for neglect at home and in the community we live in. Every man or woman is meant to look after each other in times of need.

WHAT BIRTHDAYS MEAN
“We never knew what happened on the day we were born. But it was documented. And we believe that someone took care of us, because we are here today.”
Happy New Year everyone! With a new year comes a new birth. We are filled with optimism for what is in store. Perhaps, we can also look back on our own birthdays and rethink our lives and goals.
It was a day we never knew, but it is part of us. On that day, we came into this world, helpless human beings, totally dependent on those around us for continued survival. We made it through those times until we reached independence.
Anyone who has had a chance to take care of someone who is totally dependent knows what kind of responsibility it entails. The caregiver can no longer plan for themself alone. In fact, there is a selfless disregard for one’s own needs and wants in order to fulfill another person’s requirements. Food, sleep, and recreation will all be sacrificed to find joy in helping other human beings reach their potential. The realization of the potential may take years, but it is worth the wait.
We never really knew what was happening during those first few years of our life. I lived in a day and time when taking photos was reserved for special occasions, unlike today. Technology and the internet have enabled some to document daily life events, complete with photo and video coverage, for the future adult to probably appreciate. Nevertheless, the circumstance of helplessness is similar. We had to put our trust in adults during those early days. They could have left us alone, but we were nurtured.
Our birth and death are intertwined events. On the day someone dies, someone is born too. We exist in a continuum, but it has an end, which will signal someone else’s beginning. Throughout time, those who are alive today have been affected in some way by those before them. The baby boomer who took care of a Gen X infant may have passed on experiences that now influence how the Gen Xer takes care of Generation Z. There may have been some changes depending on how one perceives the future. The Gen Xer may have resented the discipline of Baby Boomer parents, who were nurtured by very strict Pre-war parents. Thus, the Gen X adult will make adjustments to make sure the Gen Z child does not have a similar experience.
To say that a new year, or a new birth, will mean new experiences and changes is predictable. But those changes are shaped by the past. And that past may have had a perceived ending, but it actually lives on.
Birthdays mean that because we are here, we have to make the most out of what we are. We must be grateful to those who helped us in the past. And we must make an effort for those who are already nearing the exit, for we will get there too. But while we are here, we lay the foundation for the continuum of care and nurturing.
We trusted those who took care of us when we started. When we reach the end, we hope we have planted the seeds for us to be cared for when we reach the end of our days.
A FOOD GUIDE FOR THE HOLIDAYS
Enjoy the food, but never overindulge.
It’s Holiday Season again! From parties to get-togethers, family reunions, and corporate events, we have learned to enjoy this moment after the pandemic – despite the return of traffic congestion and the inevitable Christmas rush. The sociable human has found a way to return to its old ways, dancing through the extravagance and merrymaking with the hope of having something left over for the New Year.
Celebrations are not complete without food. But as in everything, one must practice moderation. There is a term coined by medical practitioners called Holiday Heart Syndrome. This refers to the arrhythmia experienced by those binging on alcohol during these times. The heart exhibits atrial fibrillation, an abnormal rhythm that can result in death. This can happen even in those individuals who have no history of heart disease.
Another dietary habit that we must observe is proper hydration. We forget that water is still the best fluid for keeping us hydrated. Sugary drinks may be more palatable, but these may overwork our vital organs such as the liver and kidneys particularly if we have diabetes or impaired glucose tolerance. Thirst may also be manifested as hunger, so being hydrated reduces our desire to eat.
Raw foods, while palatable for some, poses its dangers, particularly if its sources are unknown. Cooking reduces the possibility of food contamination, so if one prefers to eat uncooked food, it must be ensured that it is prepared well. In buffet tables, there is always the risk of spreading food-borne diseases particularly if food is not kept hot or cold. It would be an advantage to come early to the buffet table, when most diners have not yet partaken of the feast.
To create good balance in one’s meal, two to three servings of green leafy vegetables and fruits daily is a must. Fruits and vegetables are packed with essential nutrients, and have less calories. As in most cases, if one is not a vegetable eater, you could start small, with side salads added to at least one meal and go on from there. While high-protein foods increase satiety, the high fat content could possibly be a problem especially when it comes to cardiovascular risk.
Finally, make sure to go easy on refined sugars. Desserts are aplenty, and it is easy to gorge on these as they can increase meal satisfaction. However, the risk of obesity and Type 2 Diabetes lurks in the horizon. I never advise my patients against eating sweets – in fact, I am not one to restrict food groups altogether. What is more important is moderation, taking in small portions, and enjoying food.
It is not a good idea to spend time in an emergency room during the holidays. Not only is it potentially congested – the doctors manning the posts at this time are usually newbies as the experienced physicians are on vacation. So if you can avoid it, avoid the hospital at all costs.
Lifestyle diseases are preventable and modifiable.
Enjoy the holidays! And never forget the true reason for the season. Celebrate and share, for to truly eat live, and be merry, we must satisfy others, not just ourselves.
REFERENCES:
Tonelo D, Providência R, Gonçalves L. Holiday heart syndrome revisited after 34 years. Arq Bras Cardiol. 2013 Aug;101(2):183-9. doi: 10.5935/abc.20130153. PMID: 24030078; PMCID: PMC3998158.
Photo courtesy of Dr. Raymond Cruz
A COLLABORATION OF HOPE
Compassion has no start and no end. It is a continuing process whose effect is felt for generations to come.
“To cure sometimes, to relieve often, to comfort always.” This famous quote came from the late 19 th century as coined by Edward Livingston Trudeau, founder of the famed tuberculosis sanitarium at Saranac Lake in New York's Adirondacks. It is the guiding principle for the establishment of The Ruth Foundation for Palliative and Hospice Care (TRF). We may not be able to save all patients, but there is a constant service we can provide – comfort and care.
In its humble beginnings nearly ten years ago, TRF partnered with its surrounding community in Muntinlupa. From geriatric patients, it also caters today to patients from all age groups. With this comes the realization that we need to expand the palliative and hospice care service. With the establishment of the Universal Health Care Law, the vision is to provide TRF’s services to all communities in the country. No one will be left behind.
Utilizing the power and reach of the internet and other technologies, TRF launched among care providers the Palliative Collab project. It aims to provide information to all palliative and hospice care providers to connect with patients. Both private and public partnerships will be enhanced so that we can become good providers of end-of-life care, and symptom management would hopefully become accessible to everyone. Care providers will be accredited, and these partners will be empowered to make the Philippines a model of compassion in the future.
The Ruth Foundation for Palliative and Hospice Care (TRF) Founder, Dr. Rumalie Corvera, discusses the vision and mission of TRF and its plans for the future.
The PalCollab project as explained by Dr. Corvera will become the prototype for the provision of palliative and hospice care. It still has a long way to go, and admittedly, it is an ambitious project. The initial 3-year timeline that includes the provision of tele-consults and volunteer networks will be expanded from its home base in Muntinlupa. The gathering of palliative care providers is an invitation to participate in the project and enkindle the compassion that has made Filipino caregivers world-renowned for their hospitality.
TRF Executive Director, Dr. Rana Mendoza, explaining the PalCollab project to the Palliative and Hospice Care providers in the Country.
Is the provision of palliative and hospice care limited to those with medical training? Dr. Mendoza mentions that the answer is no because the project will also need – among others - information technology specialists, artists who can teach crafts, administrators who can organize events, or ordinary individuals with the inclination to comfort and visit the sick. Everyone has a role to contribute to lifting the spirits of those who have health issues. The possibilities are limitless.
TRF Director for Patient Care Services, Dr. Nanette Cruz, introduces the members of the PalCollab team. It includes physicians, nurses, caregivers, social workers, pharmacists, psychological and spiritual support providers, and various volunteers and staff.
The services provided by PalCollab will include medical and nursing services, physician and institutional referrals, counseling, institutional training, medication and supplies procurement, financial sourcing, volunteer training and empowerment, and outsourcing of caregivers, among others. For more details, please visit the website www.ruth.ph/palcollab
BEREAVEMENT
Our existence is a series of gains and losses;
Celebrate both as a part of life.
For we cannot wallow in grief all the time,
Just as we must not be content with past success.
Every journey is a series of ups and downs. It is normal and automatic for us to celebrate the attainment of goals, and to highlight milestones in our lives. Just look at social media — how many posts do we see among our friends showing the birth of a child, the awarding of a degree, or the victorious podium finish in a competition? We often see positive comments on these and urge them to do more. In contrast, comments on losses and failures are short, as if we are afraid of harming sensibilities. This might discourage people from sharing these sad moments, creating a vicious cycle that may exacerbate unexpressed loneliness.
Today, The Ruth Foundation for Palliative and Hospice Care shares with us how we can deal with loss and treat it as a part of our personal growth. The program entitled “Good Grief: Healing Hearts and Communities Through Bereavement Care” highlights testimonies and experiences that will encourage us to speak up and move on. Stories of loss, survival, support, and even heroism in the midst of struggles are interspersed with beautiful anecdotes that will convince us that the inevitability of loss is an opportunity for upliftment. I saw cries with smiles, and while looking back was filled with pain, hope is never lost.
Is there a secret to good grief? Does time heal wounds? Hearing from the experience of others, there is really no definitive timetable that can be established for moving on. Pain can remain for years even if the grieving survivors have regained functionality in their lives. This tells us that it is not the complete absence of pain that is important – rather, it is the strength of character that loss instills that makes bereavement important. And in all of this, we need each other. A community that cares allows us to have the energy to physically, mentally, and emotionally deal with the challenges of change and the courage to share the learnings later on.
A number of myths were also debunked in relation to bereavement care. Suppressing the pain to heal faster was mentioned as a myth, for it actually prolongs the agony when the reason for the pain is not addressed. We may exhibit a strong front, but external manifestations of strength by showing indifference can give those around us mixed signals about how we really feel. It is not, however, mandatory that we release those emotions publicly, for we all have different ways to grieve. As long as the method of grieving does not damage or compromise one’s future, personal coping measures must be respected and honored.
Our gratitude goes to those who contributed their time and expertise to this endeavor, led by The Ruth Foundation Founder Dr. Rumalie Corvera, Director for Training Dr. Mark Joseph Mendoza, Palliative Care consultants Dr. Ara Ofina and Dr. DJ Pedro, Spiritual Care Provider Pastor Spencer Gequillana, Social worker Lira Tañamor, and Counseling Specialist Cottie Del Rosario. Executive Director Dr. Rana Mendoza spearheaded the affair, which was held at the Crimson Hotel in Alabang and shared virtually via the Zoom platform with its 41 participants.
Congratulations to The Ruth Foundation and thank you to all the participants!






















Should We Be Concerned About Profiting In Hospice Care?
The hospice care industry may not be profitable in the Philippines now, but it could potentially become a lucrative service. Must we be concerned?
In business, a quick profit is always attractive. Whatever industry you are in, the allure of easy money always exists. It may not always be moral or ethical at times – more often than not, a get-rich-quick-scheme has few big winners and more big losers. But if it is in the industry of health care, specifically hospice care, it could present serious issues.
Dr. Joan Teno of Brown University School of Public Health in the United States, whose work has focused on end-of-life care, is one of those practitioners who have raised red flags about paid hospice services. “I’m very concerned that you’re harming not only the dying patient, but the family whose memory will be of a loved one suffering because they didn’t get adequate care.”
Hospice is a relatively easy business to start. At present, not many health care businesses are into it, because payments are usually out-of-pocket, and all services that are covered by the health insurance system require hospital admission. Hospice care can be provided at home and using lower-cost health workers, who can work longer shifts. This may allow the entry of smaller hospices, launched with the intent of profiting within a few years. Coupled with the sale of pharmaceutical drugs and equipment, a hospice care provider can potentially have steady clients with a regular cash flow.
The scary thing, however, is that not all of those entering the hospice market have the best intentions.
An aging population is a huge market for hospice care, but this segment of the society can be prone to abuse. Even if someone has deep pockets, the constant drain on resources could render someone bankrupt sooner or later if expenses are not checked. There may be a need to enact new laws for these services to streamline the practice and discourage unscrupulous businessmen from racketeering.
This has been the case in certain countries where the government covers for hospice care. If oversight is limited and payouts become generous, there could be private services who will take advantage of the constant income stream. Reports show that some of these industries provide shoddy service and charge a premium. More hospice providers will accommodate inquiries and clients, but they might be unable to spend more time with patients if needed. A study found that patients in for-profit hospices see doctors less often presumably to cut costs. In an analysis of federal data from 2014 to 2017, it was noted that profit hospices were less likely to have received any hospice visits in the last three days of life.
For-profit hospices also enroll a different set of patients, preferring those likely to remain in hospice longer. Most costs are incurred in the first and last week of hospice care. Patients who enroll in hospice must undergo several assessments to develop a care plan and set their medications. In their final days, as the body begins to shut down, patients often need additional services or medications to stay comfortable. Thus, when profits become a priority, screening becomes more important.
In this regard, one of the profitable cases that a hospice care provider can have is dementia. These patients will not die soon, but they will need constant attention to improve quality of life. They are also prone to all kinds of abuse, as their limitations make them dependent on care providers. Unlike cancer patients whose remaining days may be numbered, dementia patients may survive for years with the same needs and medications. Thus, there is no need for a service provider to constantly go searching for patients. The system might become discriminatory when this becomes common practice.
One must understand that hospice care is not easy. It requires some emotional involvement and yet, you must not bring the stressor home with you on your day off. You must have the patience to wait for patients when they take medications, and yet most of them may not realize a cure. It goes against the messianic complex of some care providers – you cannot save your patient, and yet you must still care.
Hospice Care providers are here to stay, and with an aging population, we must find ways to strengthen this segment. It is not bad to make a profit along the way, as it is actually necessary to sustain the service. Non-profit organizations might not be enough to serve the needs of the populace. Let us all work together to learn more about hospice care so that we can all benefit once we or our relatives need it.
REFERENCE:
Hospice Medicare Margins: Analysis of Patient and Hospice Characteristics, Utilization, and Cost - By Carol Bazell, Melissa A. Caplen, William Coates, Pamela M. Pelizzari, and Bruce S. Pyenson (25 November 2019)
THE HAPPY ROOM PROJECT: Spreading Good Vibes, One Room at a Time
I read an excerpt about New York City in one of Malcolm Gladwell’s books, “The Tipping Point”. It was said that during his term, Mayor Rudolph Giuliani cleaned up the subways of New York in an effort to curb criminal activity in the area. Gladwell mentioned that the strategy, known as “The Broken Window Theory”, became successful because our environment influences our well-being. By cleaning up and tidying the streets, mobsters were given the message that someone was in charge of the city and was being monitored.
For Ally*, a 6-year-old patient with Spinal Muscular Atrophy, the creation of a beautiful environment epitomized the road to a better quality of life. Through the Ruth Foundation’s Happy Room Project (which began in 2013), Ally and those with chronic illnesses get the chance to see a world of beauty and color. This can make all the difference, especially for someone who is dealing with life’s challenges at such a young age.
Ally* in her Spongebob-themed “Happy Room”.
The value of a clean, organized, and aesthetically appealing environment goes beyond pleasing the senses. Just as a healthy environment improved the character of the city of New York, promoting a “happy room” instead of a drab hospital-like atmosphere can create wonders for healing. We do not just spend money on interior design for bragging rights, just as we do not just wear well-pressed and clean-smelling clothes to attract people. The dignity and self-esteem it promotes can elevate one’s mood and promotes the release of happy hormones. These emotional benefits can make a difference in the lives of people.
In a study published recently in the Health Environments Research and Design Journal, a meta-synthesis showed that there are 5 factors needed when designing a palliative and hospice care environment. These include a shared space, a safe place, a reflective place, a place for family, and a place with good aesthetics and ambiance. It is surprising that not all hospice patients desired a private room in isolation – they craved interaction. Providing access to a small garden, or even placing plants or other living creatures in a room was a big help. A nice view conducive to self-reflection also enabled patients to see through themselves and plan out things they still want to achieve. I already mentioned in a previous article how this was accomplished in Ospital ng Muntinlupa, where a palliative care unit was recently established with the renovation of rooms for hospice care4. This may be used as a template for hospitals – even public hospitals – that are contemplating having their own hospice care units.
The SSAFeR place approach** details the factors that need to be addressed when designing a palliative care environment.
Whether the goal is to suppress crime in the city or to promote care at the end of life, a happy, secure, clean, and modest environment is always a key to success. After all, when we see nature in all its splendor, we marvel at the wonders that it offers. Humanity will always be attracted to beautiful things, for it makes our existence meaningful and colorful.
*name changed for patient’s privacy
**Miller, et. Al. (2021). The Physical Hospital Environment and Its Effects on Palliative Patients and Their Families: A Qualitative Meta-Synthesis. https://journals.sagepub.com/doi/abs/10.1177/19375867211032931
The Compassionate Community Kitchen: Transcending the Meaning of Food
We always hear the words – food is medicine – and harp about the benefits of good, healthy food on health and well-being. But what if not even food can reverse or alter the inevitability of man’s existence? That’s when we become creative and alter our perspective.
Food restores dignity. And inspired by the Dignity Kitchen in Singapore, The Ruth Foundation launched THE COMPASSIONATE COMMUNITY KITCHEN (CCK), which serves authentic Singaporean dishes individually packed to underprivileged patients.
Being a Family Physician and Medical Biochemistry Professor, I have witnessed how proper nutrition can impact health, not just physically, but emotionally as well. I can probably tell with some accuracy the nutritional content of food and what it can do to the body. What is more important from a human perspective is the happiness that can be derived from a hearty meal.
Yeo Hiok Keat, founding general manager of Project Dignity, points out, “…food makes people happy.” And it is true – once the food is served and shared, it is akin to a sharing of self, of one’s humanity.
As coined by Ruth Foundation founder Dr. Rumalie “Mae” Corvera, who is a Family Physician and Palliative Care Specialist herself, a “Compassionate Community Kitchen” gives meaning to what we do in medicine. Yes, as doctors, we are licensed to heal, prescribe medications, and care for the community that supports those who are ill. But she has not forgotten the need for food, and how food improves the quality of life. She has targeted two of the most important components of compassion – providing food and providing care.
This is why CCK is integrated with the services of The Ruth Foundation. If we want to restore a sick man’s dignity, what better way to do it than give that person the basic need for sustenance. It is akin to feeding the soul, an act that transcends whatever treatment medicine provides.
As we pass through our daily challenges and think about our tasks, let us always keep in mind that we need food – not just to sustain us, but to allow us to have the strength to serve those in need. Our basic needs may be fulfilled, but once it overflows, they must naturally trickle down to those who may need more. For every mouth that is fed by the Compassionate Community Kitchen, what is extended is not just life, but an act of brotherly love. The kind of love that was extended to us by the one who brought us to life.
For orders, please call 0945-5949465.
Visit them on Facebook: Compassionate Community Kitchen
Instagram: @cocokitchen.ph





Links where the launch was featured:
A PARTNERSHIP OF HOPE
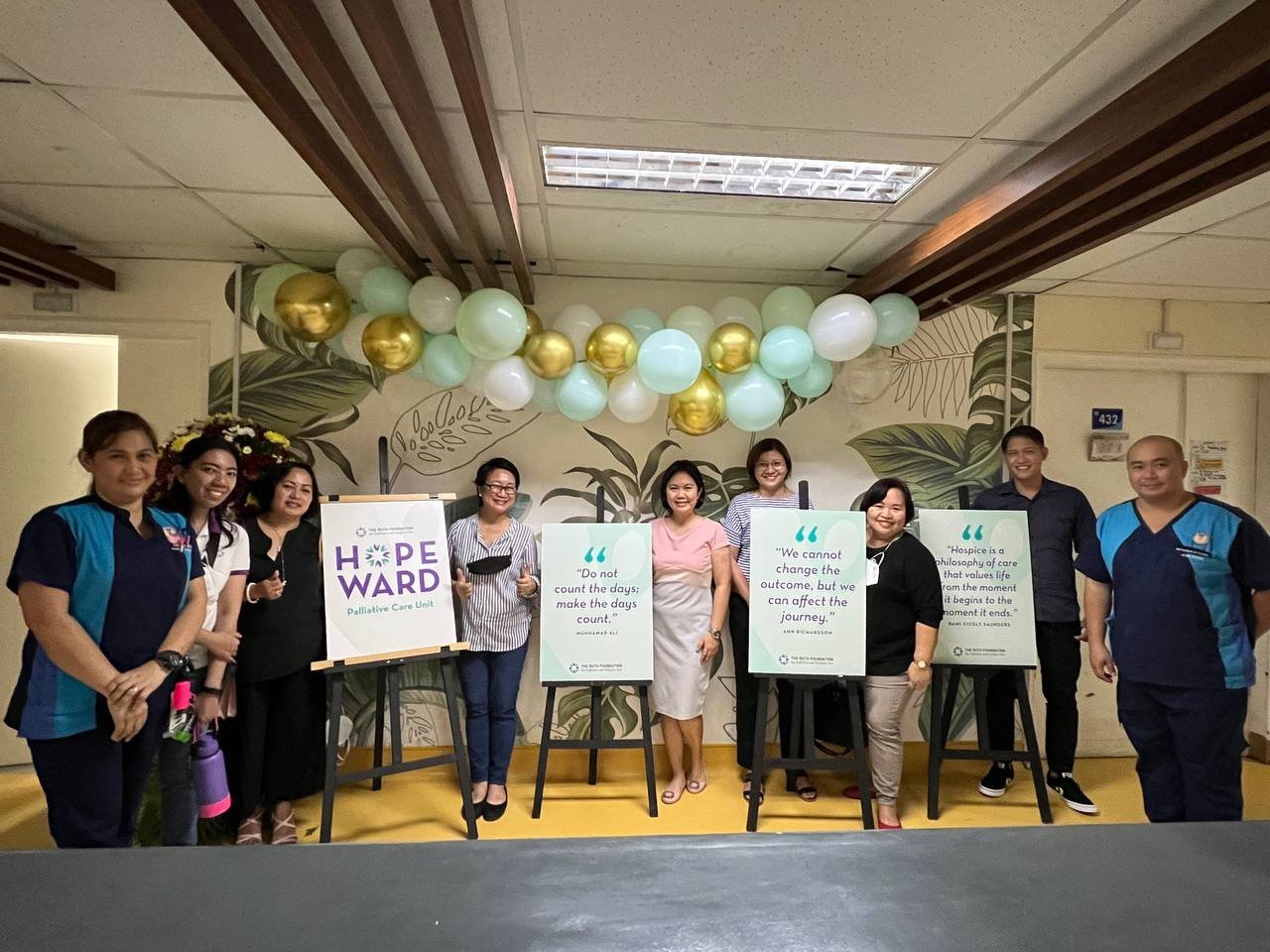
This June 30, 2022, a new ray of hope has been provided in Muntinlupa for patients needing hospice and palliative care. The new Hope Ward promises to deliver a compassionate service that will hopefully become a benchmark for all city governments. With The Ruth Foundation’s linkages with Ospital ng Muntinlupa and the City of Muntinlupa as a whole, patients needing hospice and palliative care will have access to comprehensive care from the community level all the way to tertiary level management.
As Hospice and Palliative Care continue to be recognized as an important aspect of medical management, it is necessary to provide a seamless transition from the home to the hospital when it is needed. We may have heard stories of how difficult it is, for instance, to manage pain or dyspnea at home and have the patient admitted to the hospital for symptomatic treatment. With the Hope Ward, an expert team of doctors and nurses can work hand in hand to manage urgent symptoms. A critical component that can also be addressed is education and counseling, as these stressful conditions not only produce physical manifestations. They require psycho-emotional support as well.
Congratulations to the City Government of Muntinlupa headed by Mayor Jaime Fresnedi and Congressman Ruffy Biazon, Ospital ng Muntinlupa Medical Director Atty./ Dr. Edwin Dimatatac, and The Ruth Foundation founder and CEO Dr. Rumalie Corvera. These public-private partnerships are what our country needs for the improvement of health care. And with the soon-to-open Pamantasan ng Lungsod ng Muntinlupa College of Medicine that will focus on Universal Health Care, hope springs eternal not only for the City of Muntinlupa. This promises to be a template that will be emulated by other cities in the country as well.
The 21st Century Physician
“It is no longer acceptable for a doctor to simply be a repository of knowledge; rather, and more importantly, a doctor must be able to make sense of knowledge.”
In 2004, I started my clinical practice as a newly-minted Family Medicine Specialist. I was confident, believing that I knew more than my patients. My goal then was to showcase this expertise; create impressive visual aids and prescribing materials that would show my intellectual capacity. It was how I was taught as a medical student and as a resident too. It worked —up to a point. The disconnect became obvious when I saw my patients not getting any better. It was an eye-opener.
While it is a respectable goal to instill knowledge, I realize today that I may not be the best conduit to share mere knowledge. I do not have enough time to engage with my patients in the clinical setting in order to provide extensive patient education —fortunately, the internet can make up for this deficiency. Most of the basic teachings needed for diseases can now be accessed online and can be accessed by those without a medical background. However, there is no way to replace the presence and reassuring action of a physician in patient management. There is also a need to clarify and verify whatever information is available online.
What must a physician do under circumstances such as pandemics and false information?
While I was mulling over this question, I was inspired by a bishop’s homily about The Last Supper. He emphasized three important points about the Last Supper: Humility, Availability, and Empowerment. The Lord humbled himself as a servant, and made himself available to his disciples. And during the Last Supper, he empowered his disciples to do the same. We always hear the words: “Do this in memory of me”. I think that this must also be every physician’s goal: to create a legacy that will instill a good memory of one’s efforts.
A doctor must be humble enough today to realize that he or she does not know everything. This will push the physician to continually learn and hone their craft. A doctorate degree is not the be-all and end-all of a physician – rather, it is the beginning of a long and arduous climb towards the realization of being a true healer. It is this humility that will help a doctor reach out to patients, identifying misconceptions and risky behaviors. Genuine concern is felt when a doctor is not arrogant and all-knowing. This allows the patient to freely provide relevant data.
In the age of the internet, remote communication is a blessing. This must be maximized. It might seem to be a burden to always be within reach, an email or a text message away from a patient. While this privilege may be abused, this increases patient satisfaction and compliance. There is also the advantage of having real time information about signs and symptoms, making a doctor respond rapidly in case of emergencies.
Lastly, and most important, I am most passionate about empowerment. Doctors must empower patients to take care of their health by preaching prevention rather than cure. The word “Doctor” comes from the Latin word “Docere”, meaning, to teach. We cannot deviate from it, for it is inherent in the medical profession to be a teacher in order for people to preserve their health. Part of the responsibility of being a Medical Professor is to inculcate this fact: as a doctor, you will be a teacher, and at the same time, you must empower your patients to make good health decisions. It is not a loss if the patient never gets sick, and if they do need a physician, they will not hesitate on whom to call first.
Humility. Availability. Empowerment. These are the lessons of the Last Supper. These are also the ideal traits of the doctor of the future. And I believe it will never go out of style. Just like your favorite clothes.
Non-Violence
Let us not seek to satisfy our thirst for freedom by drinking from the cup of bitterness and hatred. — Dr. Martin Luther King, Jr.
As the United States celebrated Martin Luther King Jr. Day last January 17, we are reminded of the significance of non-violent actions to initiate change. We have seen how violence can lead to significant upheavals, but in the long run it results in resentment and retaliation.
The Bible has this significant story of violent change. After the great flood during the time of Noah that destroyed everything, a covenant was established that it will never happen again (Genesis 9:11-16). This suggests that any violent action may produce immediate change, but there could be long-term consequences.
Dr. King was a powerful speaker, someone whose influence went way beyond his living years. We all impact other people’s lives, and we can make a difference. This was the sentiment of his attitude towards painful upheavals, and he realized that gentle change is more powerful in producing results.
At a time when the black people of the United States were considered as second-class citizens, his “I Have a Dream” speech resonated with everyone who has ever been bullied and discriminated upon. In medical care, this includes those who no longer have the capacity to choose treatment, those who cannot afford, and those who no longer have a good chance of survival.
Doing what is right for others must be entwined in our being. With the growing challenges of the pandemic, there still exists inequality in some fronts. Some are not able to access vaccines. Others still refuse to be vaccinated. We know that recently, even world-class athletes have been in the limelight as they insist on their own questionable beliefs. But we who believe in science plod on, continuing to pursue excellence with the dream of providing a better life for others.
Everyone can make a difference. We are influencers. Our inner circle can alter the behavior of others. Our decisions can change lives. In deciding to change behavior through gentleness and compassion, we may produce slower outcomes, but they last longer. There is no resentment afterwards.
In the Philippines, we can now see how palliative and hospice care has gone a long way in promoting human dignity. When I was a student before the turn of the millennium, a DNR in a patient’s chart meant “Do Not Resuscitate”. It also meant “Do Nothing, Really”. These patients, from being monitored on an hourly basis, were suddenly dropped like hot potatoes. Medications stopped. Visitations became less frequent. Students liked to have these patients, for there was no longer anything to carry out for them.
But through the introduction of compassionate care in the medical curriculum, the landscape started to change. There were no violent protests that led to this change. It was led through example. Then it gained ground. Today, medical futility is viewed in a different light. Medical specialists recognize its reality on all fronts. There is still some resistance, as some sectors still adhere to saving lives at all costs. But aggressive CPR is a violent way to go for the terminally ill. There is a better way to say goodbye. It lies in a silent touch, a gentle whisper, a compassionate wave.